Blog
The Swiss Cheese Model of patient safety errors: Closing the holes with message accountability
During a busy shift change several years ago, I was giving a handoff report to the oncoming nurse. We entered the patient’s room to verify his IV pump settings and attachments to chest tubes, drains, and PIVs. The patient and his wife said they had been waiting for me, which I didn’t initially understand. But then they informed me the patient had moved from the bed to the chair and accidentally disconnected his chest tube. Upon hearing this, I immediately began the necessary interventions and followed our chest tube management protocol.
The patient’s wife had used the nurse call system to reach a nurse, but whoever answered the call never relayed that message. In fact, that person may not have understood the critical nature of the situation. Luckily, the patient was fine, but I felt terrible. He should never have experienced this potentially life-threatening situation. In addition, the oncoming nurse now had more on her plate at the start of her shift to handle the paperwork. Clearly, our unit’s communication practices had some major holes that we needed to address.
What is the Swiss Cheese Model in healthcare?
The situation above is a perfect example of the “Swiss Cheese Model,” which occurs when a series of unlikely errors culminates in a catastrophe. How many times in history has disaster struck due to the Swiss Cheese Model of accident causation? From plane crashes and engineering errors to patient safety events, this model can happen in any industry.
Miscommunication often plays a significant role in these errors. In a recent analysis of 10 years’ worth of claims data, communication among providers was a risk management issue 50% of the time. The primary goal of any safe, reliable communication process is to eliminate errors, or the “holes” in the Swiss cheese.
Not all messages are equally important
While exploring how miscommunication and message accountability create these holes, it’s important to recognize that all messages in healthcare are not created equal. Telling a physician, “The family is in the room and would like to talk to you when you are free,” is different than “The CT scan shows a new, acute subdural hematoma with midline shift.” The first message is important but will likely not trigger a major change in the patient’s outcome. The second message is critical. If healthcare providers don’t urgently act on that important change in the patient’s condition, the patient will certainly have a bad outcome.
As I work with health systems and providers, I consider message accountability a way of closing the “holes” or preventing errors in healthcare communications. For Spok, message accountability is not simply the reliable transmission of a block of text from one person to another. Rather it consists of four components:
- The message contains actionable information enabling the recipient to understand the urgency and context.
- The recipient can explicitly acknowledge the message to take ownership of and responsibility for the information.
- The sender knows when the recipient has accepted accountability for the message.
- If the initial transfer of accountability fails due to lack of acknowledgment after a pre-defined time or because the message was sent to a person not responsible for acting on the information, the system will automatically escalate the message to the next appropriate individual or notify the sender.
There are numerous instances when message accountability is critical:
 Code situations
Code situations
When a patient rolls into the ED with an acute ST-elevation myocardial infarction (Code STEMI), the health system must call the cardiac catheterization team into the hospital immediately. The health system needs to know the interventional cardiologist has received the message and is on their way—otherwise, the intervention cannot happen.
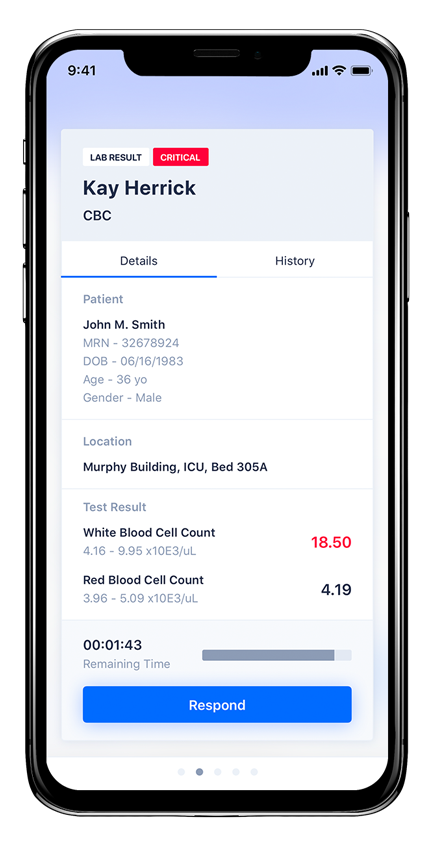
Critical test results
The subdural hematoma example above is considered a medical emergency. The radiologist diagnoses the problem but does not perform the intervention. The accountability must be transferred to the patient’s provider, and ultimately, to the neurosurgeon. In this case, the information has to be sent immediately from the radiology system with a rapid escalation path if the initial recipient does not accept accountability to ensure the patient receives the appropriate intervention quickly. (Spok Go, pictured right, has the ability to communicate and escalate results.)
Patient care Alarms
When a patient clicks the nurse call button, the request could be for water—or for help with the sudden onset of severe chest pain. The concept of message accountability ensures a responsible nurse receives the message quickly and can take the appropriate action.
As a nurse, I’m certainly aware of near misses, adverse events that occur due to miscommunication and a lack of message accountability. When care teams can’t convey messages via reliable, face-to-face conversation, Spok Go® offers an effective solution. Spok Go includes the secure messaging, interoperability with source systems, and escalation and tracking processes that go a long way toward closing potential “holes” in the Swiss Cheese Model of patient safety errors.






